Early skin cancer detection & treatment in Frankfurt
Every year, over 200,000 people in Germany are diagnosed with various forms of skin cancer such as actinic keratoses, basal cell carcinomas, squamous cell carcinomas or melanomas, making them the most common tumor disease. The good news is that both white and black skin cancer can be treated well if diagnosed early.
For the early detection of skin cancer and timely treatment, we recommend regular examinations using dermoscopy and digital dermoscopy including computer software in our practice in Frankfurt. By combining our expertise with modern diagnostic tools, we achieve significantly greater accuracy in the detection of pathological changes and can guarantee timely, gentle and safe treatment.
It is important to set individual prevention intervals based on your personal risk profile. In some cases, more frequent check-ups may be necessary. As skin cancer can also occur in young people, regular skin cancer screening is particularly important. This applies in particular to fair skin, many moles or regular sun exposure as well as a positive family history.
So it doesn’t hurt to make an appointment at our dermatology practice in Frankfurt early on.

How can skin cancer be detected?
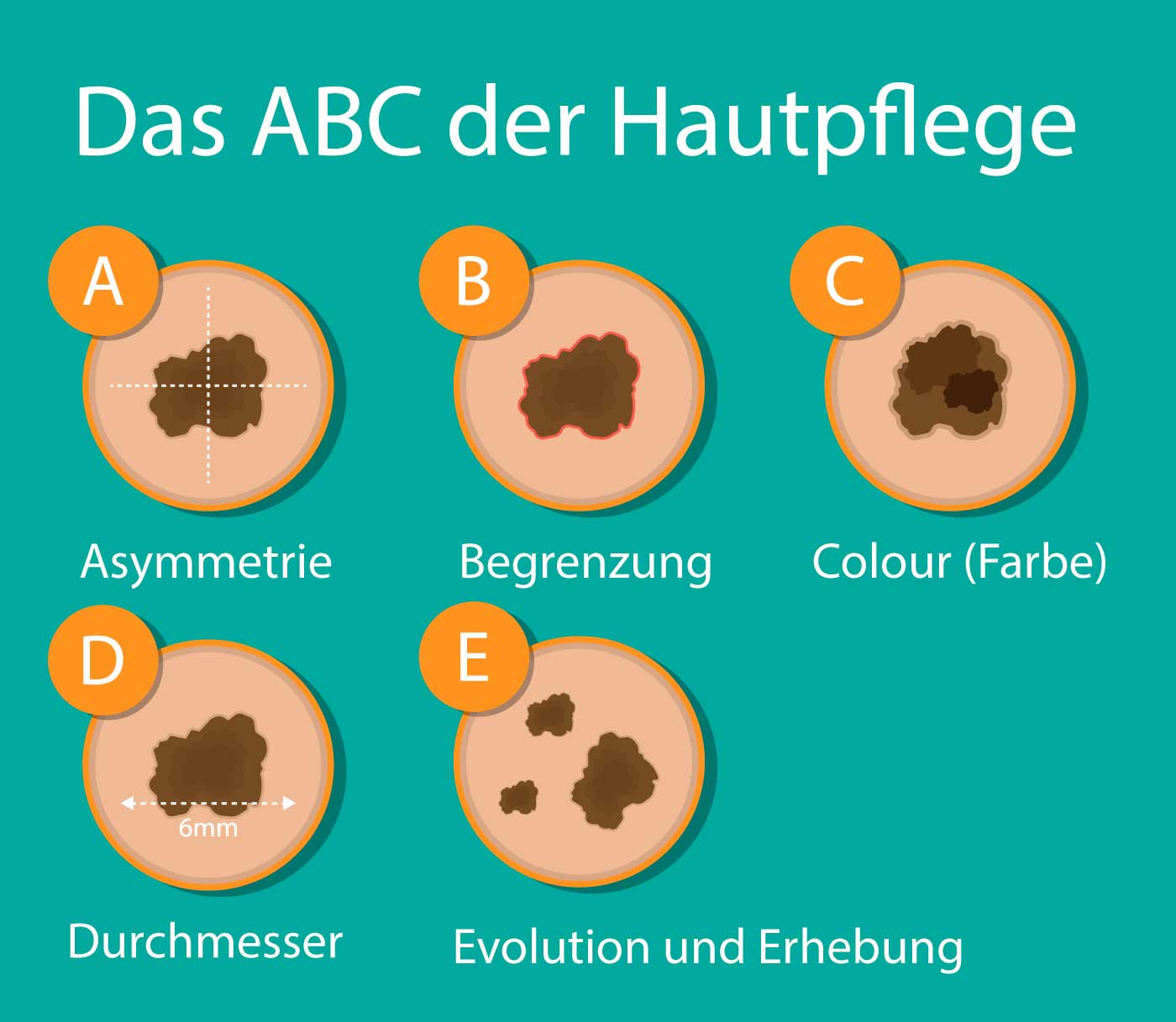
The ABCDEF rule is a useful guideline for the rough assessment or self-examination of conspicuous moles and for the early detection of skin cancer:
- Asymmetry: The pigmented mole has an irregular shape or jagged edges.
- Boundary: The edges of the pigmented mole are blurred or indistinct.
- Color: The pigment stain shows a particularly dark black coloration.
- Diameter: The pigment mole has a diameter greater than 0.5 cm.
- Evolution and elevation: The pigmented mole grows rapidly and protrudes above the skin level.
- Familial clustering: Has there been a case of melanoma in the immediate family?
It is important to note that all of these criteria may be present in a melanoma, but may also be completely absent. These rules only serve as a guide for the layman. An accurate diagnosis requires a thorough medical examination using (digital) dermoscopy. Our dermatology practice in Frankfurt can provide you with the best advice and support if you suspect skin cancer.
Types of skin cancer
Skin cancer is a tumor disease of the skin. These include melanoma, basal cell carcinoma, squamous cell carcinoma, actinic keratoses and others.
Our team of dermatologists has extensive experience in the treatment of various types of skin cancer. We offer both surgical and non-surgical treatment options and place great emphasis on holistic care for our patients throughout the treatment process.
Actinic keratoses
Repeated, short-term and intensive sun exposure over a longer period of time can cause actinic keratoses in humans (precursors of white skin cancer). Actinic keratoses particularly affect people with a light skin type on chronically sun-exposed areas such as the face, scalp, ears, neck, lower arms and lower legs.
Untreated actinic keratoses can develop into squamous cell carcinoma, a form of white skin cancer, within 5 to 10 years. An effective and gentle skin cancer treatment for actinic keratoses is laser therapy in combination with photodynamic therapy (PDT).
In this procedure, the affected area is first pre-treated with a laser and then a photosensitizer (5-aminolevulinic acid) is applied. This is followed by irradiation with red light, which triggers a photochemical process in the skin that specifically destroys precancerous lesions. This innovative therapy option offers an effective solution for the treatment of actinic keratoses, reducing the risk of developing white skin cancer. According to the Dermatology S3 guidelines, this is the best treatment option for actinic keratoses in terms of both long-lasting and cosmetic results.

Basal cell carcinoma (basal cell carcinoma)
Basal cell carcinoma (BCC), also known as “white skin cancer”, is the most common tumor disease of the skin and affects around 100,000 patients every year in Germany alone.
Risk factors for the development of BCC include excessive UV exposure and genetic predispositions, including skin type, gender and certain syndromes. Basal cell carcinoma often grows locally invasively, which means that it is limited to one area but can spread deep into the skin.
The diagnosis of BCC requires a comprehensive examination of the entire skin. Dermatoscopy can help to improve the accuracy of clinical diagnosis.
Although metastases of basal cell carcinoma are an absolute rarity worldwide, regular follow-up examinations are recommended after treatment due to the high risk of local recurrence. In the first two years after removal of the basal cell carcinoma, medical examinations are carried out every three months. After that, follow-up care is carried out every six months.
Smaller basal cell carcinomas and actinic keratoses (see above) can be treated gently and without scarring using a combination of laser and photodynamic therapy. Larger basal cell carcinomas are removed surgically and under micrographic control.
Squamous cell carcinoma (spinalioma-white skin cancer)
Squamous cell carcinoma, also known as spinalioma, is an aggressive form of white skin cancer for which repeated and intensive exposure to the sun is considered a significant risk factor.
This skin change typically occurs in people from the sixth decade of life onwards, particularly in areas that are heavily exposed to light such as the head or extremities.
A serious danger lies in its rapid growth in the depth and width of the skin. Squamous cell carcinomas must therefore be surgically removed and then examined histologically. Metastases via the lymphatic and blood vessels are a rarity.
In the first two years after removal of the spinalioma, follow-up examinations are carried out every 6 months for patients with a low to medium risk of metastasis and every 3 months for patients with a high risk, in accordance with the AWMF guidelines. This enables early detection and treatment of recurrences (recurrence of the tumor).
After a recurrence-free period of two years, follow-up examinations are carried out annually for patients with a low risk of metastasis and every 6 months for patients with a high risk in accordance with the AWMF guidelines. In the case of particularly thick squamous cell carcinomas (over 6 mm), regular ultrasound examinations of the draining lymphatic channels are also recommended.
After four years, further check-ups are individually adapted and carried out every two years at the latest.
Melanoma
Melanoma, also known as black skin cancer, is the most dangerous form of skin cancer, as the tumor originates from the melanocytes, the black pigment cells of the skin. It can either be new (de novo) or develop from existing moles.
In Germany, around 30,000 people are diagnosed with melanoma every year. If left untreated, melanoma can metastasize in the body via the lymphatic system or blood vessels.
For the early detection of skin cancer, we rely on our expertise as well as on reflected light dermoscopy and digital skin cancer screening in our practice in Frankfurt.
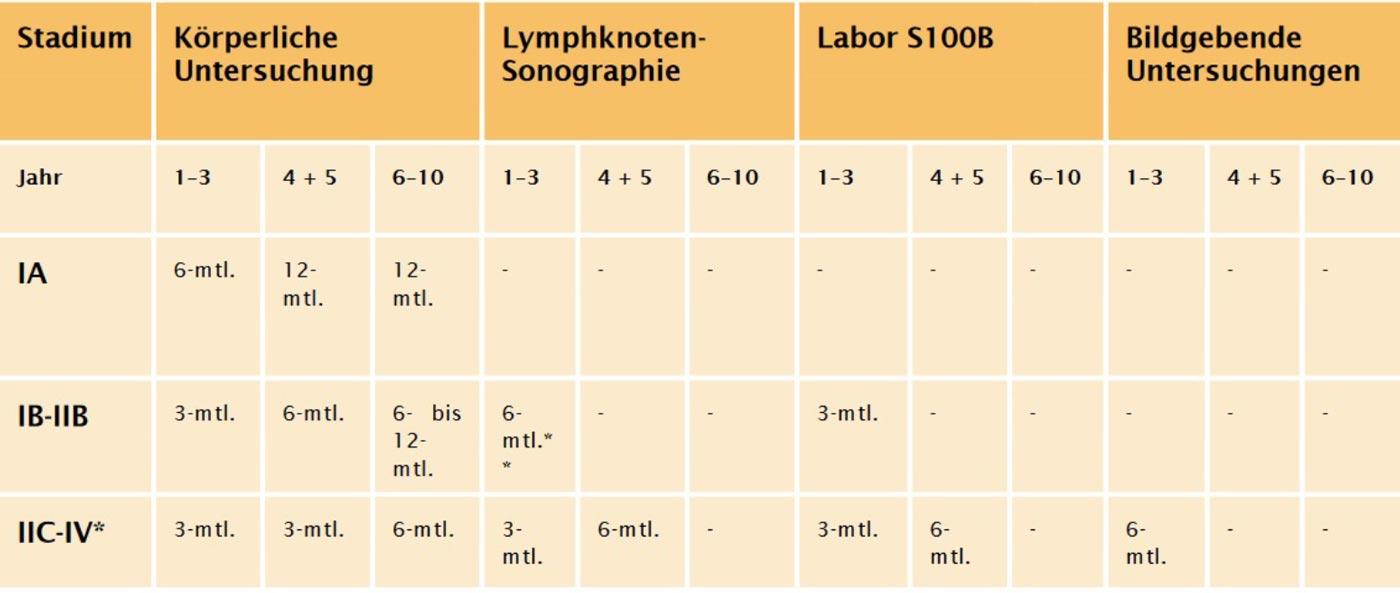
These measures allow melanomas to be detected in good time and treated using 3D surgery. Subsequently, regular follow-up examinations – depending on the stage of the disease – are of crucial importance.
Irrespective of the medical follow-up examinations, it is important that you examine your skin and body carefully and regularly for suspicious skin changes and palpate the lymph node sites and lymph channels. If you are unsure whether you see a conspicuous spot on your skin, do not hesitate to contact our dermatology practice in Frankfurt. We will be happy to help you with the slightest suspicion of skin cancer.

Skin cancer aftercare Frankfurt
After successful skin cancer treatment, regular follow-up care is of the utmost importance in order to detect and treat a possible recurrence of melanoma at an early stage.
Our team of dermatologists recommends customized follow-up examinations based on the stage of melanoma and the individual risk factors of each patient. These examinations may include a combination of clinical examination, reflected light dermatoscopy and, if necessary, imaging procedures such as ultrasound.